Adeno-associated virus (AAV) belongs to the genus of the dependent virus, subfamily of parvovirus, and is a natural-deficient single-stranded DNA virus. The wild-type AAV genome is approximately 4.7 kb and contains the rep and cap genes as well as the ITR sequences at both ends. Although humans are susceptible to AAV, no clinically relevant diseases have been found. AAV can be divided into different serotypes based on variations in the AAV capsid protein gene. Different serotypes of AAV have different tissue specificities. The interest gene was substituted for the rep and cap genes to construct a two-stage ITR vector, and the rep and cap were placed on a separate vector, and the adenovirus-assisted gene vector was used to package the gene with interest. Recombinant adeno-associated virus (rAAV).

At present, rAAV has been widely used as a gene transduction vector, and the safety of rAAV in human experiments has also been confirmed. As early as 1996, scientists chose lung as the first targeted experimental organ of rAAV. Below we aim to introduce the promoter, serotype selection of rAAV in lung experiments, and the AAV injection method in the lungs of mice.
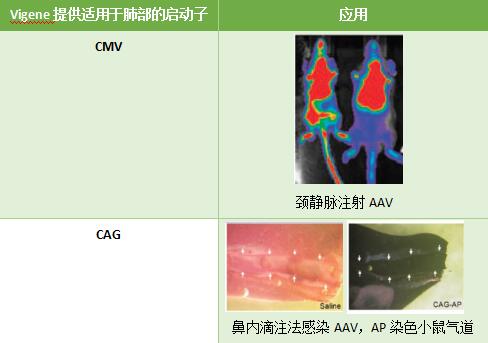
- Promoter selection
Different promoters can be selected to increase lung expression efficiency depending on the mode of injection and the purpose of the experiment. CMV is highly efficient in initiating eukaryotic gene expression and efficiently infects the lungs of mice; CAG also has excellent ability to infect airways.
- Serotype selection studies have shown that for lung infections rAAV in serum
Studies have shown that the choice of serotypes for lung infections in rAAV varies according to animal models, mainly between mice and lower primates and higher primates.
In mice and some lower primates, AAV5 and AAV6 are the best choice for infecting the lungs.
Serotype | Infected surface | Infection site and level | Receptor |
r AAV2 | The basal layer is much larger than the surface layer | Airway cells: low or no Alveolar cells: low or no Bronchial epithelium: low level or no Airway smooth muscle: medium level | Heparin Sulfate |
r AAV 5 | The base layer is larger than the surface layer | Airway cells: medium level Alveolar cells: medium level | PDGFR, 2-5 sialic acid receptor |
r AAV 6 | surface layer | Airway cells: medium level Alveolar cells: higher levels Bronchial epithelium: medium level Airway smooth muscle: low level | Sialyl glycoprotein |
r AAV 9 | Base layer and surface layer | Airway cells: low level Alveolar cells: medium level | Galactosyl dextran |
For higher primates, AAV1 is more effective in infecting the lungs; in lung cancer studies, we recommend the following AAV serotypes:
species | AAV serotype recommendation |
Mice and lungs of lower primates | AAV5/AAV6 |
Higher primate lungs | AAV1 |
Lung cancer | AAV2 (or lentivirus) |
- Mouse lung AAV injection method
There are many methods for AAV infection in the lungs. The more common methods are intranasal instillation, endotracheal intubation, and intratracheal injection. When the specific requirement for lung infection AAV is low, intravenous injection can also be used; when performing lung cancer tumor formation experiments, intratumoral injection can also be used.
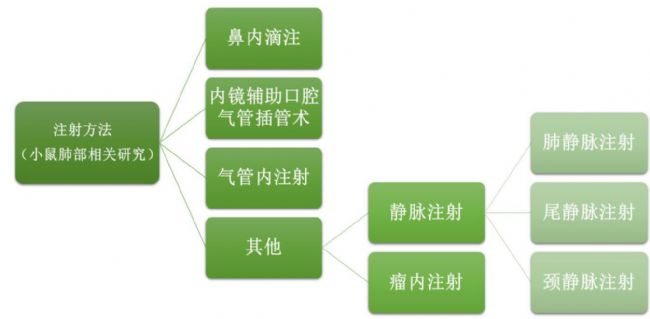
Here, we introduce the intranasal instillation, endoscopic assisted oral tracheal intubation and intratracheal injection.
- Intranasal drip
Intranasal instillation is a direct AAV infection method that is simple to operate and requires low equipment and is equally applicable to novice lab assistants. The disadvantage is that AAV particles are easily deposited in the upper respiratory tract (nasal tract, sinus and pharynx) and the gastrointestinal tract, and if a lower infection is required, a larger dose of AAV may be required.
- The mice were anesthetized by intraperitoneal injection of ketamine and xylazine;
(Animals must be in a state of deep enough anesthesia to prevent exercise or sneezing or coughing on the carrier)
(2) Fixing the mouse in a back posture on a rodent table;
(3) placing the incisor ring on the upper incisor of the mouse and attaching the Velcro to the corresponding Velcro on the lower surface of the rodent table;
(4) Slowly drip the AAV suspension through the inner wall of the mouse's nostrils. To ensure maximum lung infection efficiency, the minimum volume is 50 μL (25 μL per nostril), and the maximum volume is 75 μL (37.5 μL per nostril). ). After the mouse's breathing returned to normal, a 75 μL AAV suspension was added dropwise;
(5) gently remove the mouse from the workbench and raise the head and chest with a folded tissue to ensure a smooth breathing of the mouse;
(6) After the mouse wakes up, put it back into the cage.
- Endoscopic assisted oral tracheal intubation
Oral tracheal intubation allows the viral vector to be directly administered into the lungs without the risk of surgery and the loss of viral particles from the upper respiratory tract. Since almost all AAV virus particles reach the lungs, the amount of AAV used is strictly controlled. At the same time, oral tracheal intubation requires some special equipment compared to intranasal drip infusion, and it is slightly more difficult to operate.
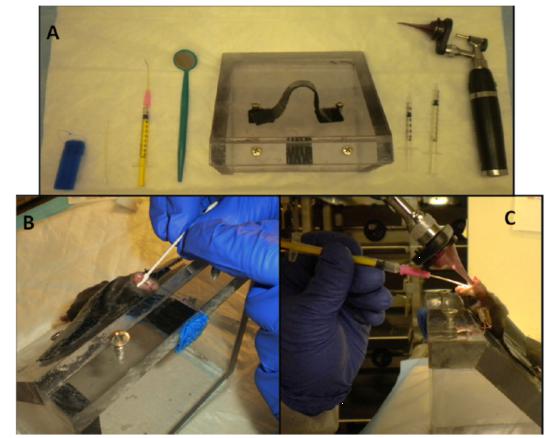
- The mice were anesthetized by intraperitoneal injection of ketamine and xylazine;
(Animals must be in a state of deep enough anesthesia to prevent exercise or sneezing or coughing on the carrier)
- The mouse is fixed in a back posture on a rodent table;
- Place the incisor ring on the upper incisor of the mouse and attach the Velcro to the corresponding Velcro on the lower surface of the rodent table;
- The back of the mouse should be completely flat on the workbench, the chest should not be biased to the sides, and the nylon buckle should be completely fixed;
- Roll up the mouse's tongue with a pointed cotton swab;
- Gently insert the cannula with the otoscope into the tracheal opening in the deep throat (approximately at the front of the ear). The concave surface of the cannula should be away from the tongue;
- Gently move the otoscope until you can see the throat (sometimes you need to rotate the mirror slightly to get the best view); you should pay attention to the small range of motion. If you only see the back of the tongue, you need to remove it again and start from the beginning;
- When the throat can be seen, a drop of 2% lidocaine can be added, and the cannula can be removed (less than 30 s) before intubation, during which the catheter needle is positioned;
- After 30 seconds, repeat steps (3) - (5), re-insert the intubation mirror, and find the position where you can see the throat;
- After the throat can be seen again, the catheter needle first enters the tracheal opening. After the needle is in place, the cannula can be removed, and then the catheter is slowly lowered until the center of the catheter (pink part) contacts the mouse incisors, each small Do not try to insert the catheter more than 2 times;
- Once the catheter is in place, remove the needle so that the mouse can breathe normally;
- Determining the correct position of the catheter within the trachea;
- Use a 0.35 mL syringe through the catheter to enter AAV at 3 μL / g body weight;
- Immediately use a 1 mL needleless syringe to input 0.2 mL of air and repeat 2-3 times to reduce the residual AAV in the catheter;
- Remove the catheter;
- The mice were gently removed from the table and the head and chest were gently raised with folded paper towels to ensure smooth breathing of the mice;
- The state of the mouse is monitored until it wakes up and it is expected that mild to moderate breathing will be restored within 24 to 36 hours.
- Intratracheal injection
Compared with intranasal instillation, intratracheal injection can increase the efficiency of AAV into the lungs; compared with oral tracheal intubation, the device is simpler and easier to operate. At the same time, endotracheal injection has a very high risk of surgery, including bleeding, incision cracking, infection, and a longer recovery period. Not only that, because the mouse's trachea is narrow, it is also prone to mistakes, AAV injection into the peri-tracheal tissue or esophagus.
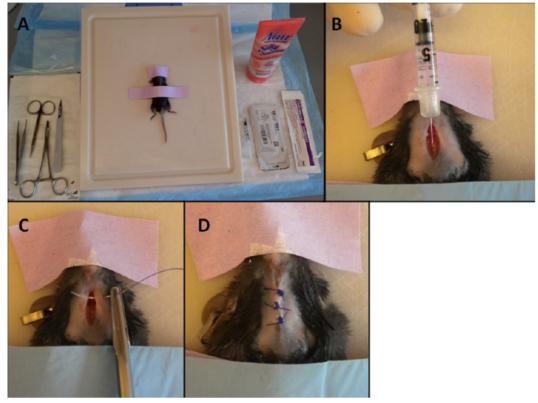
- The mice were anesthetized by intraperitoneal injection of ketamine and xylazine;
(Animals must be in a state of deep enough anesthesia to prevent exercise or sneezing or coughing on the carrier)
- The mouse was fixed in a back posture on a rodent table, the chin and the four front ends were fixed, and the mouse was slightly raised on the 45° slope;
- Remove the hair from the ventral side of the mouse neck (from the throat to the chest);
- Use a damp gauze sponge to clean the hair removal area, then wipe the skin with a chlorine-containing solution, and finally wipe with 70% alcohol;
- Cut a 4 mm incision in the upper part of the neck of the mouse;
- Use the tissue to gently pass through the subcutaneous tissue to find the trachea covered by the cervical band muscle;
- Exposing the trachea with a light incision on the band muscle;
- Once the trachea can be seen, insert the needle obliquely upward into the trachea, point the needle to the lungs, enter AAV at 3 μL/g body weight, and then pull the needle out;
- Stitching the incision or bonding with skin glue;
- The mice were gently removed from the table and the head and chest were gently raised with folded paper towels to ensure smooth breathing of the mice;
- The state of the mouse was monitored until it awakened.

Clinic Nitrile Gloves,Nitrile Gloves Small,Medical Gloves Unsterilized,Nitrile Gloves Powder Free Latex Free
Puyang Linshi Medical Supplies Co., Ltd. , https://www.linshimedical.com